Rugalmas. Integrált. Biztonságos.
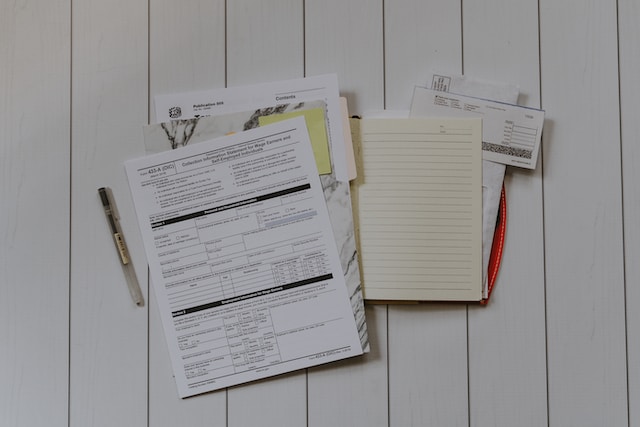
LIBRA vállalatirányítási rendszerek az operatív és adminisztratív tevékenységek, valamint a vezetői döntéshozatal támogatásához

LIBRA 3s
integrált ügyviteli rendszer kis- és középvállalkozásoknak
- Rugalmas folyamattámogató megoldás
- Teljes körű adatszolgáltatás
- Kedvező díjszabás

LIBRA 3s
integrált vállalatirányítási rendszer nagyvállalatoknak
- Átfogó vezetői kontroll
- Teljes integráltság
- 100%-os biztonság

LIBRA Online Számla
LIBRA Online Számla
- ERP vagy fájl szintű integráció
- Valós idejű, automatizált online adatszolgáltatás
TÁRJA FEL A LEHETŐSÉGEIT
Szabja cégére a LIBRA rendszereket speciális funkciókkal és kapcsolódó megoldásainkkal.
LIBRA Folyamat- menedzsment
LIBRA Folyamat- menedzsment
LIBRA Report Engine
LIBRA Virtua
Személyszállítási szoftvermegoldások
Személyszállítási szoftvermegoldások
LIBRA InfoCenter
Közüzemi szoftvermegoldások
Közüzemi szoftvermegoldások
LIBRA-EKÁER kapcsolat
LIBRA Projektkalkuláció
LIBRA Projektkalkuláció
SZAKMAI
TAPASZTALAT
a vállalatirányítási rendszer terén
A Libra Szoftver Zrt. 2006-ban jött létre a Volán Elektronika Zrt. leányvállalataként. A LIBRA az anyavállalattól az integrált vállalatirányítási és ügyviteli szoftverek forgalmazását és utógondozását vette át, melyek a néhány fős kisvállalkozásoktól egészen a több ezer főt foglalkoztató nagyvállalatokig, a legkülönfélébb környezetben és a gazdaság minden területén, a non-profit szférában és az oktatásban is alkalmazásban vannak.
Szoftverek, amelyek együtt növekednek a céggel
A partnerségben hiszünk.
Minden adat egy helyen.
AMIT KÍNÁLUNK
Egyetlen program vagy komplex rendszer – Ön dönt!
Teljes integráltság
Nincs szükség többszörös adatbevitelre, és mivel az egyes funkciók egymásra épülnek, az adatok egy egységes vállalati adatbázisba kerülnek.
100%-os biztonság
Az adatbázis-kezelő rendszer eredendően biztosítja a tranzakciók védelmét – adatvesztés vagy programhiba miatt adatvisszatöltési igény még nem fordult elő.
Széles körű lekérdezési lehetőség
Tetszőleges listák és kimutatások készíthetők minden programból.

Rugalmas méretezhetőség
A rendszerek moduláris felépítésűek, így könnyedén az igényekhez alakíthatóak.
Gyártói támogatás
Folyamatos szoftverkövetés biztosítja, hogy a LIBRA rendszerek mindenben naprakészek legyenek.
Felhasználóbarát, egyszerű működés
Az egyedi igényeket cégre szabott fejlesztésekkel szolgáljuk ki.
AHOL KIEMELKEDŐEK VAGYUNK
Speciális iparági csoportok, ahol a LIBRA rendszerek évtizedek óta támogatják a vállalat működését.
Közműszolgáltatók
Volán társaságok
Városgazdálkodók
Erdőgazdaságok
ESETTANULMÁNYOK
Partnereink, akikkel régóta osztozunk a sikerben
CÉGÜNK
A Libra Szoftver Zrt. az elmúlt években cégcsoporttá nőtte ki magát.






AMIRE BÜSZKÉK VAGYUNK
Partnereink véleménye a LIBRA rendszerekről